Wisdom teeth, or third molars, usually appear between the ages of 17 and 25. However, they don’t always bring wisdom. Often, they bring problems.
According to a 2024 global meta-analysis, 36.9% of individuals (and up to 43.1% of individuals in Asian-sample studies) had at least one impacted third molar. This suggests that among Asians, a significant proportion may carry impacted wisdom teeth.
Understanding when wisdom tooth removal is necessary can save you from severe pain and costly emergency dental procedures. Singapore dental clinics emphasise that early recognition of warning signs allows for planned surgical extraction during optimal healing periods.
In this article, you’ll understand the seven key warning signs that can help you make informed decisions about your oral health and avoid the complications that come with delayed treatment.
Key Takeaways
- Watch for warning signs early. Persistent pain, swelling, recurring infections, or difficulty chewing may indicate problematic wisdom teeth.
- Early intervention reduces complications. Addressing wisdom teeth before severe impaction or infection makes extraction simpler and recovery faster.
- Professional assessment is key. Digital X-rays and thorough dental exams help plan the safest removal and protect surrounding teeth and nerves.
- Maintain oral health post-extraction. Follow aftercare instructions carefully to prevent infection, ensure smooth healing, and protect your smile.
1. Persistent Pain and Throbbing in the Back of Your Mouth
Persistent pain at the back of your mouth is one of the most telling signs that your wisdom teeth may require attention. Dentists frequently observe that ongoing discomfort behind the molars, especially when it intensifies over time, can indicate impacted wisdom teeth pressing on the surrounding bone and adjacent teeth.
How does this pain feel?
- Typically, a deep, dull aching sensation, different from a regular toothache
- Often starts intermittently but gradually becomes more frequent and intense
- Frequently described as a constant throbbing that can disrupt sleep and concentration
The pain frequently radiates beyond the immediate tooth area, extending to the jaw, ear, or neck region. This radiation occurs because the trigeminal nerve, which supplies sensation to the face, can transmit wisdom tooth pain to distant areas.
Pain that persists despite over-the-counter pain medication often indicates infection and severe impaction, which requires surgical extraction.
Dentists stress that ignoring persistent wisdom tooth pain can lead to more serious complications, including damage to neighbouring teeth, cyst formation, and extensive bone loss that complicates future extraction procedures.
2. Swelling and Inflammation of Gums
Red, swollen, or bleeding gums around emerging wisdom teeth are often a sign of pericoronitis, an inflammation (and possibly infection) of the gum around a wisdom tooth that hasn’t fully erupted through the gums. This condition is commonly seen in patients requiring wisdom tooth removal.
What happens and why?
- Bacterial buildup: Partially erupted wisdom teeth can create pockets beneath the gum flap (operculum) where bacteria accumulate.
- Localised inflammation: The gum around the wisdom tooth becomes red, swollen, tender, and warm, and may bleed easily during brushing or eating.
- One-sided effect: Usually affects one side of the mouth first, unlike general gingivitis.
Swelling around wisdom teeth can extend beyond the immediate gum area to the cheek or jaw region. In a 2024 case report, a 66-year-old man developed a deep facial and jaw abscess caused by a decayed upper wisdom tooth. Such infections are life-threatening and require urgent hospital treatment, surgical drainage, and intravenous antibiotics.
Dentists emphasise that recurrent gum inflammation around wisdom teeth rarely resolves with conservative treatment alone. While acute episodes may temporarily improve with professional cleaning, antibiotics, and improved oral hygiene, insufficient space for the third molar typically necessitates surgical extraction to prevent future episodes.
3. Recurring Infections and Bad Breath
Chronic infections around wisdom teeth are strong indicators that extraction may be necessary, especially when accompanied by persistent bad breath, unpleasant taste, or repeated episodes of pericoronitis (gum inflammation).
Dentists note that these recurring infections often occur because the deep, hard-to-reach location of third molars creates ideal conditions for bacterial buildup.
Why do infections keep coming back?
- Food and debris accumulation: Partially erupted wisdom teeth often trap food under the gum flap (operculum), creating an anaerobic environment where harmful bacteria thrive.
- Bad breath and taste: Bacterial growth produces volatile sulfur compounds, causing bad breath localised to the back of the mouth. Patients often notice a persistent unpleasant taste, which may indicate the presence of pus even if it’s not visible.
- Limited relief from hygiene measures: Regular brushing and mouthwash usually cannot eliminate this odour or taste because the infection is trapped beneath the gum flap.
These infections can present with swelling and tenderness around the gums and, sometimes, fever when the infection becomes systemic.
Dentists also have observed that persistent halitosis (bad breath), especially when it’s concentrated around the back molars, can often be linked to issues with wisdom teeth, even if patients initially seek help for general halitosis.
4. Difficulty Opening Your Mouth or Chewing
Limited jaw opening, medically called trismus, often accompanies wisdom tooth problems and is a significant warning sign. Inflammation from infected or impacted wisdom teeth can extend into the muscles of mastication, especially the medial pterygoid muscle, leading to restricted mouth opening and painful chewing.
This difficulty usually starts on one side, as patients unconsciously avoid chewing on the affected area. Initially mild, the restriction can worsen as inflammation spreads.
Key symptoms of trismus related to wisdom teeth:
- Difficulty opening the mouth fully (often not wider than two fingers’ width)
- Painful chewing on the affected side
- Morning jaw stiffness that improves throughout the day
- Swelling or tenderness near the back molars
- Difficulty speaking, swallowing, or, in severe cases, breathing
Dental specialists consider persistent or worsening trismus a red flag for deep space infection. In severe cases, it can compromise the airway, making it a potential medical emergency. Any difficulty swallowing, speaking, or breathing, along with trismus, requires immediate professional evaluation.
5. Crowding and Shifting of Other Teeth
Eruption of wisdom teeth can cause noticeable changes in dental alignment, especially in patients who previously underwent orthodontic treatment.
Crowding usually becomes most visible in the front lower teeth, where patients notice previously straight incisors beginning to overlap or twist. This late lower incisor crowding develops gradually, often starting subtly before becoming cosmetically concerning.
For patients who invested in braces during their teenage years, seeing their smile change despite prior orthodontic success can be particularly frustrating.
Pressure from wisdom teeth often occurs when they lean forward against the second molars (mesial angulation). This can:
- Shift the second molars out of position
- Affect the root structure of adjacent teeth
- Create tight contact points that are difficult to clean, increasing the risk of decay between teeth
That’s why general dentists frequently recommend preventive wisdom tooth extraction for patients who have completed orthodontic treatment. Removing problematic wisdom teeth helps preserve orthodontic alignment and prevents future complications that may require additional corrective treatment.
The bite changes caused by wisdom tooth pressure can extend beyond simple crowding. When third molars affect how the upper and lower teeth come together, or cause misalignment of nearby teeth, extraction is strongly advised to prevent progressive damage to the overall dental arch.
6. Frequent Headaches and Jaw Pain
Tension headaches and jaw pain often accompany wisdom tooth problems. Impacted wisdom teeth can cause chronic muscle tension throughout the head and neck, leading to persistent headaches that patients may not immediately associate with their teeth.
The mechanism involves the jaw muscles and the trigeminal nerve system. When wisdom teeth cause pain or bite irregularities, patients often unconsciously clench or grind their teeth, particularly during sleep. This constant muscle tension radiates through the temporal, masseter, and neck muscles, creating headache patterns.
Morning headaches are especially common, caused by overnight clenching or grinding in response to dental pain, combined with jaw fatigue from avoiding wisdom tooth discomfort.
Common symptoms of headaches and jaw issues related to wisdom teeth:
- Tension headaches that worsen in the morning
- Jaw stiffness and soreness
- TMJ (temporomandibular joint) symptoms, including clicking, popping, or locking
- Pain radiating to the temples, neck, or surrounding facial muscles
- Headaches resembling tension headaches or migraines due to referred pain
Dental specialists emphasise that persistent headaches and jaw pain, especially with TMJ symptoms, may indicate impacted wisdom teeth that require professional evaluation.
7. Impaction Visible on X-ray (Even Without Symptoms)
Not all problematic wisdom teeth cause noticeable pain or discomfort right away. Sometimes, issues are hidden beneath the gums, and the first warning sign is visible only on a dental X-ray.
Dentists use panoramic or digital imaging to detect impaction, which occurs when a wisdom tooth is unable to fully erupt due to a lack of space, obstruction by other teeth, or abnormal angulation.
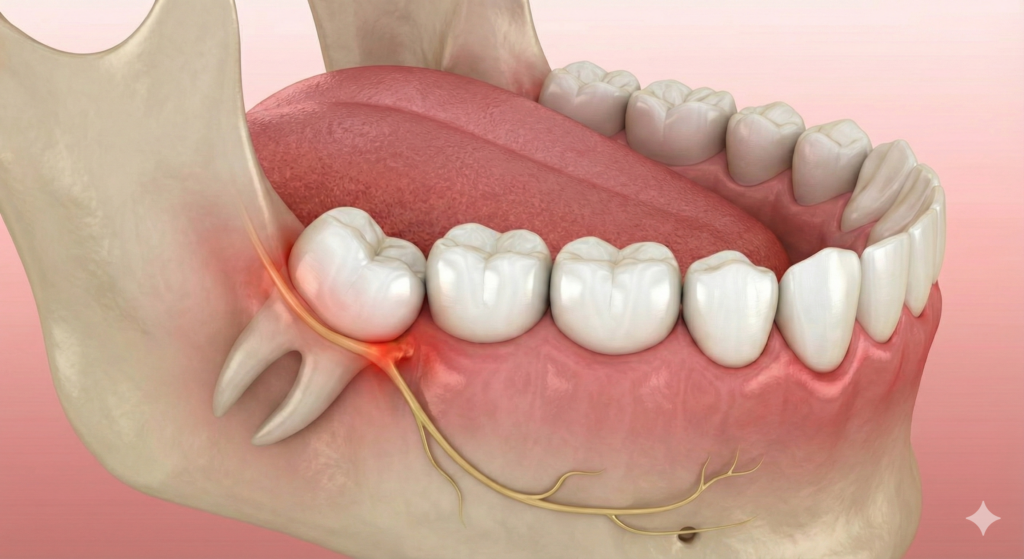
Common types of impaction include:
- Horizontal impaction: The wisdom tooth lies sideways and pushes against the second molar.
- Mesial impaction: The tooth angles forward toward the front of the mouth, pressing on adjacent teeth.
- Vertical impaction: The tooth remains partially trapped in the jawbone, unable to emerge properly.
Even if you don’t feel pain, impacted wisdom teeth can:
- Damage neighbouring teeth by exerting pressure or causing decay
- Create pockets where bacteria accumulate, increasing infection risk
- Contribute to cyst formation in rare cases
Dentists often recommend early extraction of impacted wisdom teeth detected on X-rays to prevent future complications.
When to Consult a Dentist
Immediate dental consultation becomes essential when experiencing multiple symptoms such as:
- Multiple warning signs at the same time
- Pain that interferes with daily activities
- Swelling that extends beyond the tooth area
Many dental experts recommend monitoring wisdom‑tooth development during the late teens and early twenties because complication rates and recovery times increase with age.
What Your Dentist Will Typically Do Next
When you visit your orthodontist for concerns about wisdom teeth, the goal is to carefully assess the teeth, manage any active infection, and plan the safest extraction, if needed. The approach usually involves a combination of examination, imaging, and treatment planning.
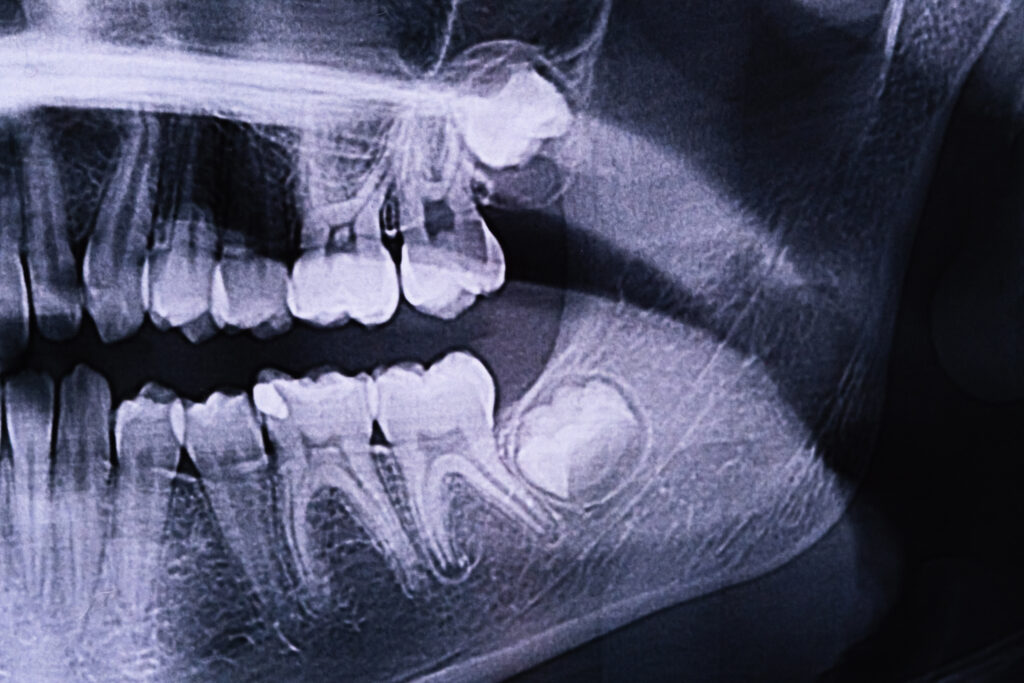
Clinical Exam + X-ray (OPG)
Dentists start with a thorough dental examination combined with digital imaging to evaluate:
- Position and angulation of the wisdom teeth
- Bone structure surrounding the teeth
- Relation to critical areas such as the inferior alveolar nerve and maxillary sinus
An orthopantomogram (OPG) X-ray provides a full view of all four wisdom teeth and helps dentists determine whether extraction is necessary and how complex it might be.
Conservative Steps (if appropriate)
For patients with acute infection but otherwise manageable wisdom tooth positioning, dentists may initially:
- Prescribe antibiotics
- Recommend warm saltwater rinses
This approach helps reduce inflammation and allows the area to heal before deciding if extraction is required.
Extraction Options
The type of extraction your dentist recommends depends on how your wisdom teeth have developed and whether they are causing problems.
- Simple extraction: Suitable for fully erupted, easy-to-reach wisdom teeth. Performed under local anaesthesia, this procedure usually has minimal recovery time.
- Surgical removal: Required for impacted or partially erupted teeth. This procedure may involve:
- Cutting the gum tissue
- Removing some bone
- Sectioning the tooth
- Stitches and temporary facial swelling
Addressing wisdom teeth early generally results in simpler procedures, faster healing, and better outcomes.
Note: Some complex cases may need general anaesthesia and a more comprehensive procedure. Hence, the cost, recovery time, and aftercare of a wisdom tooth removal in Singapore vary.
Wisdom Tooth Removal in Singapore: Why Acting Early Matters
If you notice persistent pain, swelling, recurring infections, difficulty chewing, or changes in your teeth alignment, these are strong signs that wisdom tooth removal may be necessary. Early recognition of these warning signs allows for simpler procedures, faster recovery, and fewer complications.
At Elements Dental, our experienced dentists provide safe, comfortable, and professional wisdom tooth removal in Singapore using modern techniques tailored to each patient.
Don’t wait until pain or infection becomes severe. Book a consultation with Elements Dental today and take the first step toward a healthier, pain-free mouth.